Closing The Loop on Patient Engagement: Overcoming the PA Washout
Dan Rubin discusses how a full-service prior authorization (PA) support program facilitates higher PA submission rates and more prescriptions dispensed.
Pharma brands invest heavily in sales and marketing tactics aimed at convincing physicians to prescribe their product. Even when successful, these efforts represent only a first step in realizing more prescriptions that actually get dispensed. Particularly when a prescription requires prior authorization (PA), retail pharmacy data shows that the originally prescribed product ends up being dispensed less than thirty percent of the time[1]. In two-thirds of cases, the medication is either switched to another product or abandoned altogether, leaving both patients and physicians frustrated. PA requirements are being implemented by payers for more brands across most therapeutic categories, so the negative impact on pharma continues to deepen.
As pharmaceutical marketing has evolved from “selling pills” to assuring that medications actually get dispensed and taken by patients, many brands have layered patient engagement and support programs into the marketing mix to assist with a range of issues including patient education, therapeutic support, benefit verification, financial assistance, and adherence support. Many brands utilize a patient support program (sometimes referred to as a “patient hub”) as a single point of contact for patients to access these support services online or via 800 numbers. Beyond receiving general product/condition education prior to therapy initiation, patients frequently use these support programs to verify insurance coverage, understand whether prior authorization is required, obtain co-pay cards, or explore the potential availability of Medicare tier exceptions[2].
While patient support programs often claim to address patient access issues such as PA, they usually fail to result in high physician submission and approval rates. After performing a patient-specific benefit verification and determining that a PA is required, the typical action is to fax a PA form to the prescriber. Similarly, if the patient is covered by Medicare and might be eligible for a lower co-pay from a tier exception (TE), they typically fax the Medicare Coverage Determination form to the practice. In either case, practices frequently do not follow through on the PA or TE request due to the burdensome submission and follow up process required by the managed care (or Medicare) plan. As a result, the PA doesn’t get submitted and the patient gets switched to an alternative therapy or abandons treatment altogether.
One brand utilized an innovative program to drive more prescriptions by integrating a full-service PA support program based on the result of their benefit investigation. When a patient inquired about benefit coverage for the brand, and it was determined that the patient’s plan required a PA, the patient support program forwarded the patient/plan/physician information to the service provider, who then created a substantially-completed PA form in their web-based Prior Authorization Support System (PASS). Physicians were notified that the patient had inquired about their coverage for the product, and that a PA was required. The physician was informed that they could access the substantially-completed PA by entering a proprietary access code in PASS to complete the PA submission. Once submitted, the service provider managed the PA process on behalf of the physician, including follow up calls to the managed care plan as required and notification of the plan’s decision on the PA. Reminder communications were provided to physicians who did not submit the PA after receiving the initial notification.
Prior to implementing this new program, the brand reported that physician PA submission rates were very low and when a PA was submitted, approval rates averaged around 50-60 percent.
Results. After implementing the new program, the brand saw significant increases in both PA submission and approval rates. Physicians submitted PAs more than 50 percent of the time after receiving a notification from the service provider. Over 42 weeks, physicians submitted a total of 952 PAs independently (without receiving any notifications). After receiving notifications, physicians submitted an incremental 4,967 PAs, with a 75 percent average approval rate.
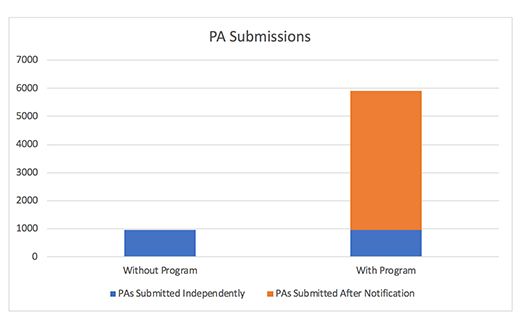
Overall, the program resulted in nearly 4,000 incremental approved PAs, which translated into approximately 10,000+ incremental TRx’s. The brand’s return on investment in the program was sixteen to one, and more importantly, approximately 4,000 patients ended up receiving the medication their physician deemed best, instead of a substitute therapy or abandoning therapy altogether.
When left on their own, many practices will not deal with the cumbersome process of completing and submitting PAs. A service that makes this process more streamlined and less time consuming for physicians and their staff will lead to higher PA submission rates and more prescriptions dispensed.
Many pharma brands have already created patient support programs that address patient coverage issues. Adding an effective PA service can be a small incremental step that yields large benefits from more patients on therapy, less physician frustration, and fewer prescriptions being substituted or abandoned.
Dan Rubin is President and CEO of PARx Solutions.
[1] Point of Care Partners. Electronic Prior Authorization for Medications: The Time is Right for Plans, PBMs and Other Payers. February 2012, Hanson KA. Journal of Managed Care Pharmacy. An Analysis of Anti-Hypertensive Use Following Initially Rejected Pharmacy Claims for Aliskiren. September 2009. Vol. 15, No. 7. pp. 573-574
[2] A tier exception involves a physician submitting a “Coverage Determination form” requesting that the patient’s co-pay is reduced to a lower formulary tier.
Pfizer, GSK Gain ACIP Recommendations for RSV and Meningococcal Vaccines
April 18th 2025The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices voted to expand access to Pfizer’s respiratory syncytial virus vaccine Abrysvo for high-risk adults in their 50s and voted in favor of GSK’s meningococcal vaccine, Penmenvy, for streamlined adolescent protection.
Navigating Distrust: Pharma in the Age of Social Media
February 18th 2025Ian Baer, Founder and CEO of Sooth, discusses how the growing distrust in social media will impact industry marketing strategies and the relationships between pharmaceutical companies and the patients they aim to serve. He also explains dark social, how to combat misinformation, closing the trust gap, and more.