
The move is part of Synaptogenix’s partnership with Cannasoul.

A Harvard Business School Healthcare Alumni Association Q&A with Louis Kassa, CEO of the Pennsylvania Biotechnology Center.

The latest news for pharma industry insiders.

The pharmacy will now operate as Saveway Compounding Pharmacy, a Myonex company.

Collaboration aims to advance the development of treatments for multiple neurodegenerative conditions, including amyotrophic lateral sclerosis.
A combination of data from the EMERGENT-4 trial and pooled data from the EMERGENT program showed the promise of KarXT (xanomeline-trospium) in providing symptom improvement for people with schizophrenia.

These expansions include a new product, along with improvements to existing products.

The latest news for pharma industry insiders.

Dovato is the first oral, two-drug, single-tablet regimen approved for patients 12 years of age and older who are living with HIV-1.

According to the letter, the FDA believes that the investigational apomorphine infusion device is not ready for approval in its current form.
PIONEER AF-PCI exploratory trial found that elderly patients experienced a lower rate of clinically significant bleeding after 12 months of treatment with Xarelto (rivaroxaban).
The approval of AstraZeneca’s and Daiichi Sankyo's Enhertu (trastuzumab deruxtecan) for adults with unresectable or metastatic HER2-positive solid tumors adds to the drug's approved indications in breast cancer, non-small cell lung cancer, and gastroesophageal junction adenocarcinoma.

The latest news for pharma industry insiders.

The deal, which is worth approximately $13.1 billion, is part of J&J MedTech's goal to expand into high-growth markets.

Decision to discontinue marketing authorizations for Relyvrio/Albrioza comes as a result of topline results from the Phase III PHOENIX trial in patients with amyotrophic lateral sclerosis.

Abecma was found to triple progression-free survival compared to standard regimens with a 51% decline in the risk of disease progression or death in patients with relapsed or refractory multiple myeloma who were previously administered two or more lines of therapy.

FDA’s program will provide guidance to the development of the company’s Delphi-MD technology.

The technology will reportedly improve consumer engagement.

The vaccine can reportedly prevent infection from a fungal source that impacts both people and dogs.

The latest news for pharma industry insiders.
Early results have demonstrated that mRNA-3927 has led to a 70% reduction in the relative risk for metabolic decompensation events in patients with propionic acidemia.

Agreement comes as Teva aims to strengthen its biosimilar portfolio as part of its "Pivot to Growth" strategy.

The two programs will be offered to students and CVS interns.

Otsuka and Click Therapeutics co-developed Rejoyn, a digital therapeutic for MDD.

The latest news for pharma industry insiders.

Fanapt was previously approved by the FDA in 2009 as an antipsychotic treatment for schizophrenia.
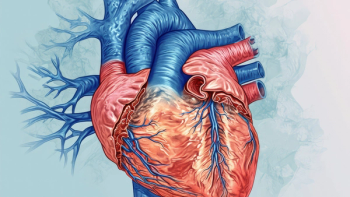
Approval comes amid positive results from TRILUMINATE trial, which demonstrated improvement in 90% of participants treated for a leaky tricuspid heart valve.

A Q&A with Dr. Zeynep Ton, professor at the MIT Sloan School of Management.

The latest news for pharma industry insiders.

The two company’s will provide consumers with a platform where they can compare drug prices.